Summary
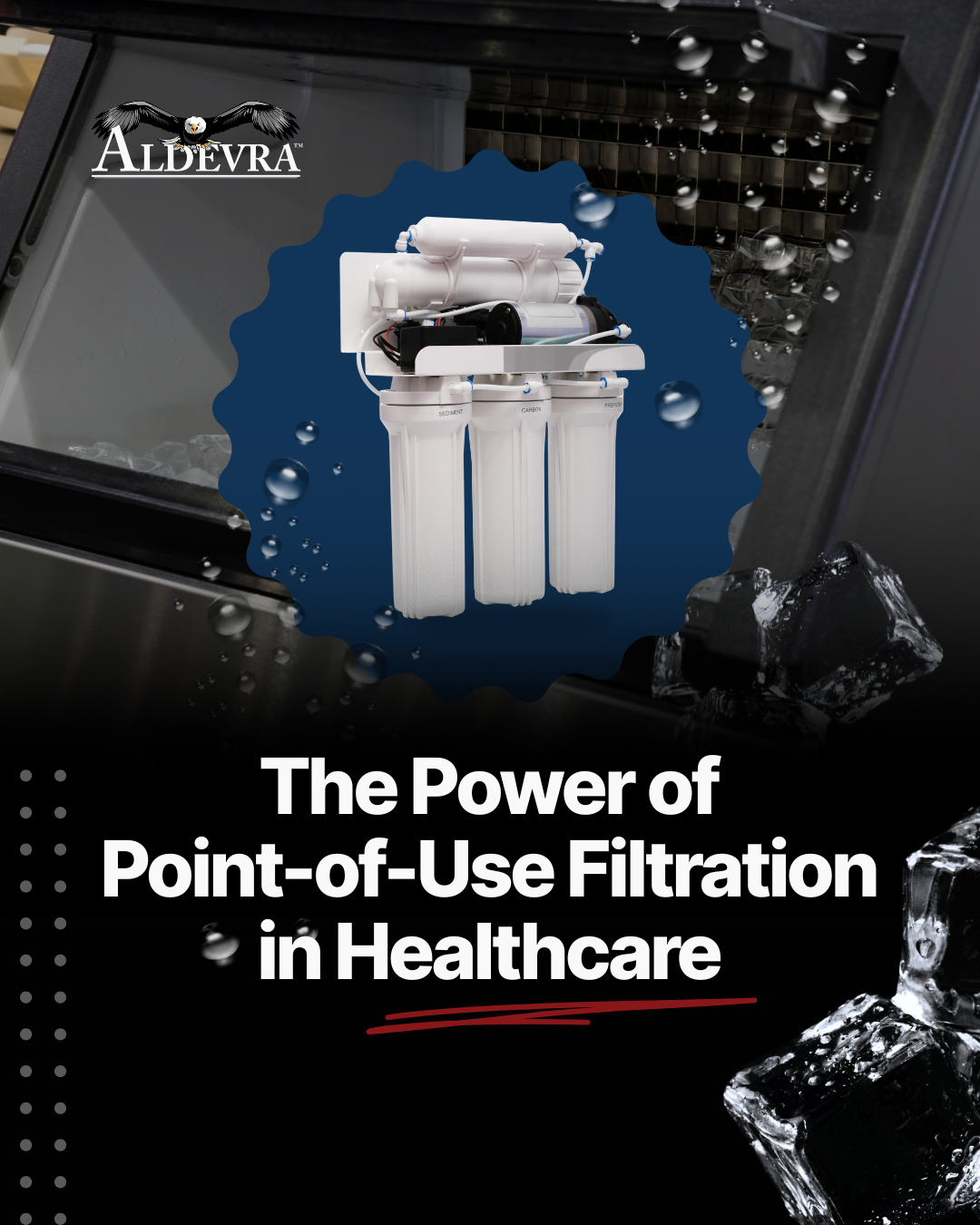
Point-of-use filtration is one of the simplest and most effective ways to protect patients from waterborne pathogens in healthcare facilities. Learn how point-of-use filters work, where to install them, and what standards guide their use.
Why Point-of-Use Filtration Matters
In a hospital or clinic, water touches nearly everything — from handwashing and food prep to medical procedures and ice machines. When that water carries bacteria like Legionella, Pseudomonas, or Mycobacterium, it can lead to serious infections, especially in immunocompromised patients.
That’s why point-of-use (POU) filtration has become a frontline defense in healthcare water safety programs. Instead of relying solely on centralized treatment, a POU filter provides protection exactly where water is used — at the outlet.
What Is Point-of-Use Filtration?
“Point-of-use” simply means filtration installed at the last possible point before water is dispensed — for example:
- Faucets and showers in patient rooms
- Ice machines and beverage dispensers
- Dialysis stations or procedure sinks
Each filter acts as a physical barrier, removing microorganisms and debris that might have survived upstream disinfection or grown in the building’s plumbing system.
How It Works
Most healthcare-grade point-of-use filters use a 0.2-micron absolute membrane — fine enough to block bacteria like Legionella pneumophila and Pseudomonas aeruginosa.
A two-stage setup is common:
- Pre-filter (5–10 microns): Captures sediment, rust, and scale.
- Bacterial-retentive filter (0.2 microns absolute): Prevents pathogens from entering the equipment or outlet.
In ice machines, this configuration ensures the water feeding the unit is clean and stays disinfected.
Standards That Support Point-of-Use Filtration
Healthcare water safety isn’t guesswork — it’s guided by national standards and regulations:
- ASHRAE Standard 188 – Requires risk management plans for Legionella control.
- CDC Toolkit – Provides step-by-step guidance on implementing those plans.
- VA Directive 1061 – Mandates use of validated point-of-use filters in patient-care areas as part of Legionella prevention.
- NSF/ANSI 53 & 58 – Certification for filters proven to reduce bacteria and cysts.
These standards agree: point-of-use filtration is an accepted and proven engineering control. Read more about these standards here
Maintenance and Best Practices
Like any safety device, POU filters only work if maintained properly:
- Replace pre-filters every 6 months or sooner if flow slows.
- Replace bacterial-retentive filters every 6–12 months or after disinfection.
- Document each change in your Water Management Plan.
- Always follow the manufacturer’s instructions for sanitation and flushing.
For ice machines and similar equipment, the recommended preventive maintenance sequence is:
- Change bacterial-retentive filter – Always replace the final filter first to ensure downstream sterility.
- Pressurized water sanitize – Flush internal plumbing lines with a pressurized, EPA-registered sanitizer (200 ppm), ensuring contact through the outlet.
- Change pre-filter – Replace the upstream sediment pre-filter to remove particulate buildup and protect the new final filter.
- Clean and descale – Use manufacturer-approved cleaning agents to remove scale and biofilm from the ice machine and associated tubing.
- No-rinse sanitize – Apply a final, no-rinse sanitizer to the ice bin, evaporator, and food contact surfaces before resuming operation.
Why this order matters:
Performing filtration steps before sanitization prevents biofilm or debris from migrating downstream during cleaning. Performing cleaning and descaling after pressurized sanitization reduces chemical load through the filters and helps maintain bacterial control.
Cost-Effective and Scalable
Installing a point-of-use filter is one of the fastest, most affordable ways to improve water safety. It’s especially useful for smaller facilities or those with aging plumbing that can’t easily support large-scale disinfection systems.
Start with high-risk areas — ICUs, oncology wards, and procedure rooms — and expand as resources allow. Even one POU filter per outlet can dramatically lower risk.
Key Takeaways