Summary
Keeping patients safe isn’t just about cleaning surfaces. It’s also about the water that feeds sinks, showers, and your ice machines. A smart testing plan tells you if your controls and filters are working — before there’s a problem.
Why water testing matters
- Legionella and other germs can grow inside complex hospital plumbing.
- Testing proves your hot/cold temps, disinfectant, and filter setup are doing their job.
- Results guide corrective actions (flush, sanitize, replace a filter, adjust temperature, etc.).
- It’s a core part of a Water Management Plan (WMP) aligned with ASHRAE 188 and the CDC Toolkit.
Where to test in a healthcare facility
Think “source → system → patient areas → endpoints.” Start here:
Building-Level
- Incoming water (baseline quality)
- Hot water loops (at least one per loop)
- Storage tanks / heaters (outlet)
Patient-Care Areas (highest priority)
- ICU, oncology, transplant, long-term care
- Ice machines and ice/water dispensers (upstream of filter, downstream of final bacterial-retentive filter, and ice from the bin)
- Showers and faucets in units serving high-risk patients
Support & Procedure Areas
- Dialysis, respiratory therapy, burn units
- Pharmacy clean rooms (as applicable)
- Kitchen/foodservice (less clinical risk, still important for hygiene and taste)
Quick rule: If water will touch patients (directly or indirectly), or equipment that touches patients, add it to your testing map.
What to test (keep it focused)
A. Microbiological
- Legionella (culture or validated method): confirms microbial safety
- HPC (heterotrophic plate count): trends general microbial load
- Coliform/E. coli (as needed): screens for contamination events
B. Chemical/Physical
- Disinfectant residual (free chlorine or monochloramine): shows ongoing protection
- Temperature (hot and cold): Legionella thrives in lukewarm water
- pH, hardness, TDS: prevents scale/corrosion that can shelter biofilm
- Iron & manganese (if staining or taste issues appear)
How often to test (sensible cadence)
VA facilities: align your cadence with VHA Directive 1061(4). The structure above fits that intent.
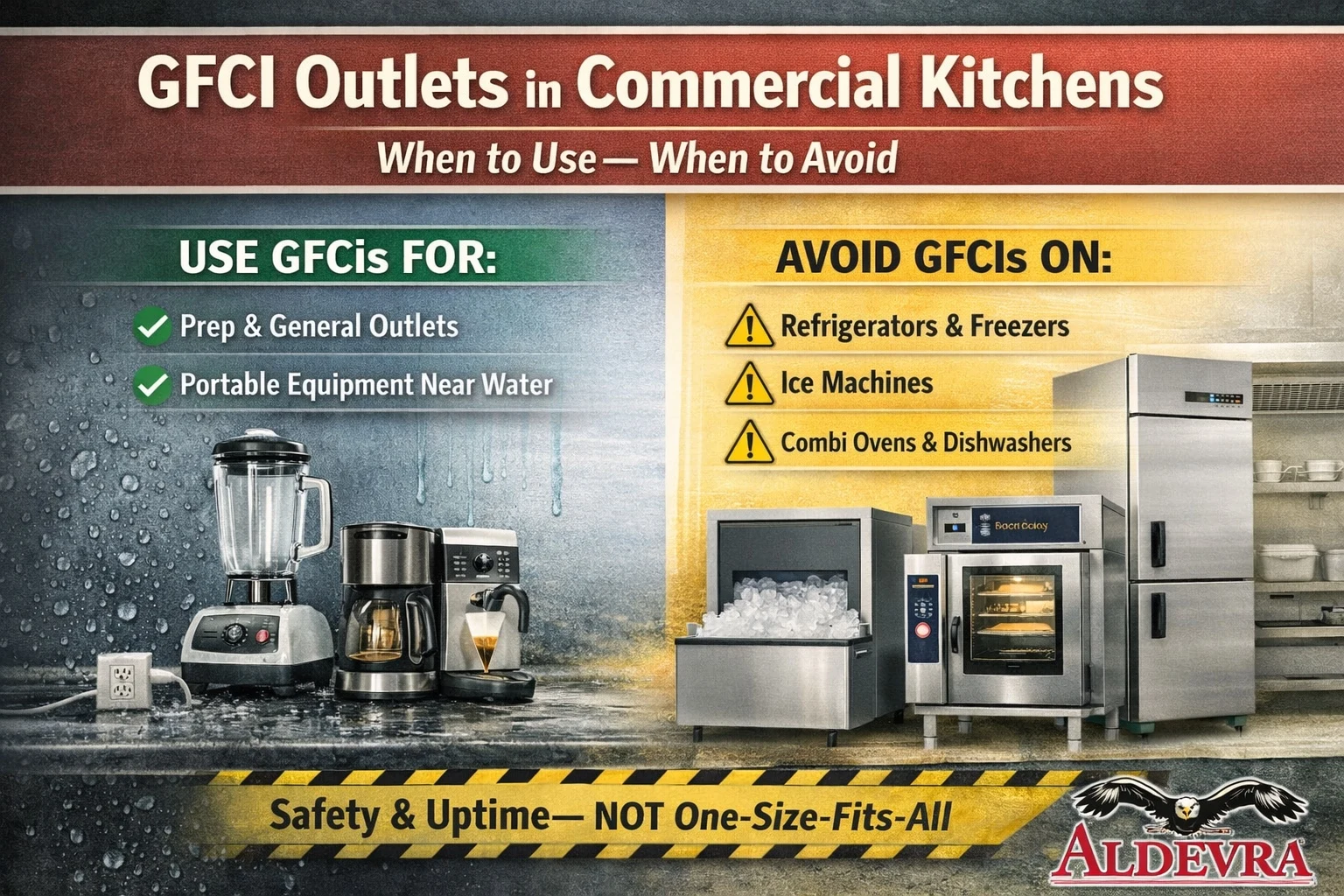
Ice machines: special attention
Your ice machine is a known risk point in healthcare. Pair testing with the right filter setup:
- Two-stage filtration:
- Carbon-less sediment pre-filter (5–10 µm) – keeps disinfectant intact
- 0.2 µm “absolute” bacterial-retentive filter – the last barrier before the machine
- Sample points:
- Upstream of filters (incoming quality)
- Downstream of final bacterial-retentive filter (verify barrier)
- Ice from the bin (end-product safety)
•PM order (every service): final filter → pressurized sanitize → pre-filter → clean & descale → no-rinse sanitize
How to collect samples (simple best practices)
- Use clean, labeled bottles (lab-provided if possible).
- Take microbiological samples first, before any chemical tests or flushing.
- Don’t sample right after chemical disinfection unless you’re verifying the result (follow lab guidance).
- For ice, use a clean scoop into a sterile bag, avoiding bin surfaces.
- Keep samples cold and deliver to the lab promptly (follow holding times).
What to do with results (decision tree)
Within limits & negative tests → Keep current schedule; document.
Low disinfectant or warm cold-water temps → Increase flushing, adjust valves, fix mixing issues, recheck in 24–72 hrs.
Scale/corrosion indicators rising → Review softening/pretreatment; descale equipment; inspect filters and pressure drops.
Positive Legionella → Follow your WMP: pressurized sanitize lines, replace filters, increase flushing, consider temporary point-of-use outlets restrictions, retest per policy. Repeated positives? Evaluate secondary disinfection (e.g., chlorine dioxide or copper–silver ionization).
The simplest documentation that still works
Keep a one-page log per location (machine/outlet). Record:
- Date & location
- Parameter (temp, disinfectant, Legionella, etc.)
- Reading & limit
- Status
- Corrective action (if needed)
- Initials
Aldevra offers a free Ice Machine Testing & Monitoring Log Tool you can embed or link. It auto-saves entries, exports to PDF/Excel, and makes survey time easier.
Budget-friendly rollout (good → better → best)
Good: Test quarterly for microbiology in high-risk areas; weekly temps; monthly disinfectant; keep logs. Ensure each ice machine in patient areas has a carbon-less pre-filter + 0.2 µm absolute filter.
Better: Expand testing to more locations; add pressure gauges/quick-connect heads to speed filter changes; add staff refreshers.
Best: Add secondary disinfection building-wide (e.g., chlorine dioxide), plus sensors that track temps and residuals; integrate dashboards with your WMP.
FAQs
Do I still need to clean if I have great test results and filters?
Yes. Filters reduce what gets in; cleaning/descaling removes what grows inside.
Is UV enough by itself?
No. UV doesn’t leave a residual. Keep your 0.2 µm absolute filter at the ice machine and follow your PM routine.
Where do I start if we’ve never tested?
Map patient-care areas first, sample ice machines and nearby outlets, set weekly temp and monthly disinfectant checks, and add quarterly Legionella testing.
Quick checklist to get going this week
- List all ice machines and high-risk outlets
- Confirm two-stage filter setup on patient-care machines
- Start weekly temp and monthly disinfectant checks
- Schedule quarterly Legionella tests (begin with high risk)
- Launch simple logs (one page per location)
- Train staff on ice handling and reporting
Bottom line
A clear water testing plan — focused on ice machines, smart filters, and a few routine checks — lowers risk fast and gives you proof during audits. If you want help, contact Aldevra.